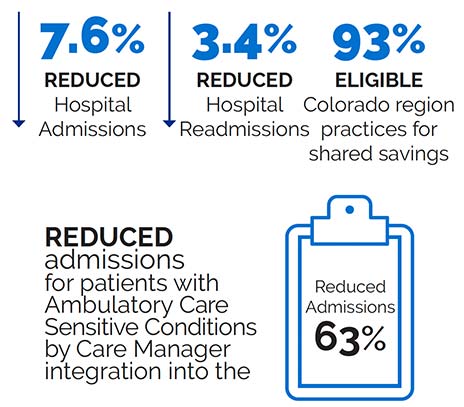
The Comprehensive Primary Care (CPC) initiative was a four-year multi-payer initiative designed to strengthen primary care. Since CPC’s launch in October 2012, CMS has collaborated with commercial and State health insurance plans in seven U.S. regions to offer population-based care management fees and shared savings opportunities to participating primary care practices to support the provision of a core set of five “Comprehensive” primary care functions.
These five functions are:
- Risk-stratified Care Management
- Access and Continuity
- Planned Care for Chronic Conditions and Preventive Care
- Patient and Caregiver Engagement
- Coordination of Care across the Medical Neighborhood
The initiative tested whether provision of these functions at each practice site — supported by multi-payer payment reform, the continuous use of data to guide improvement, and meaningful use of health information technology — can achieve improved care, better health for populations, and lower costs, and can inform future Medicare and Medicaid policy.
CPC serves as the foundation for Comprehensive Primary Care Plus (CPC+), a five-year advanced primary care medical home model launched in 14 regions in January 2017.
HealthTeamWorks' Role
During the CPC Initiative, HealthTeamWorks provided quality improvement coaches to 62 practices over the course of two years. HealthTeamWorks facilitated shared learning through learning collaboratives and on-site coaching support. Other components of the program included: data reporting and registry functionality, practice team redesign support, system and workflow redesign, advanced access, and practice culture. HealthTeamWorks also provided national technical assistance through facilitation of national webinars, EHR affinity groups and rapid cycle action groups.